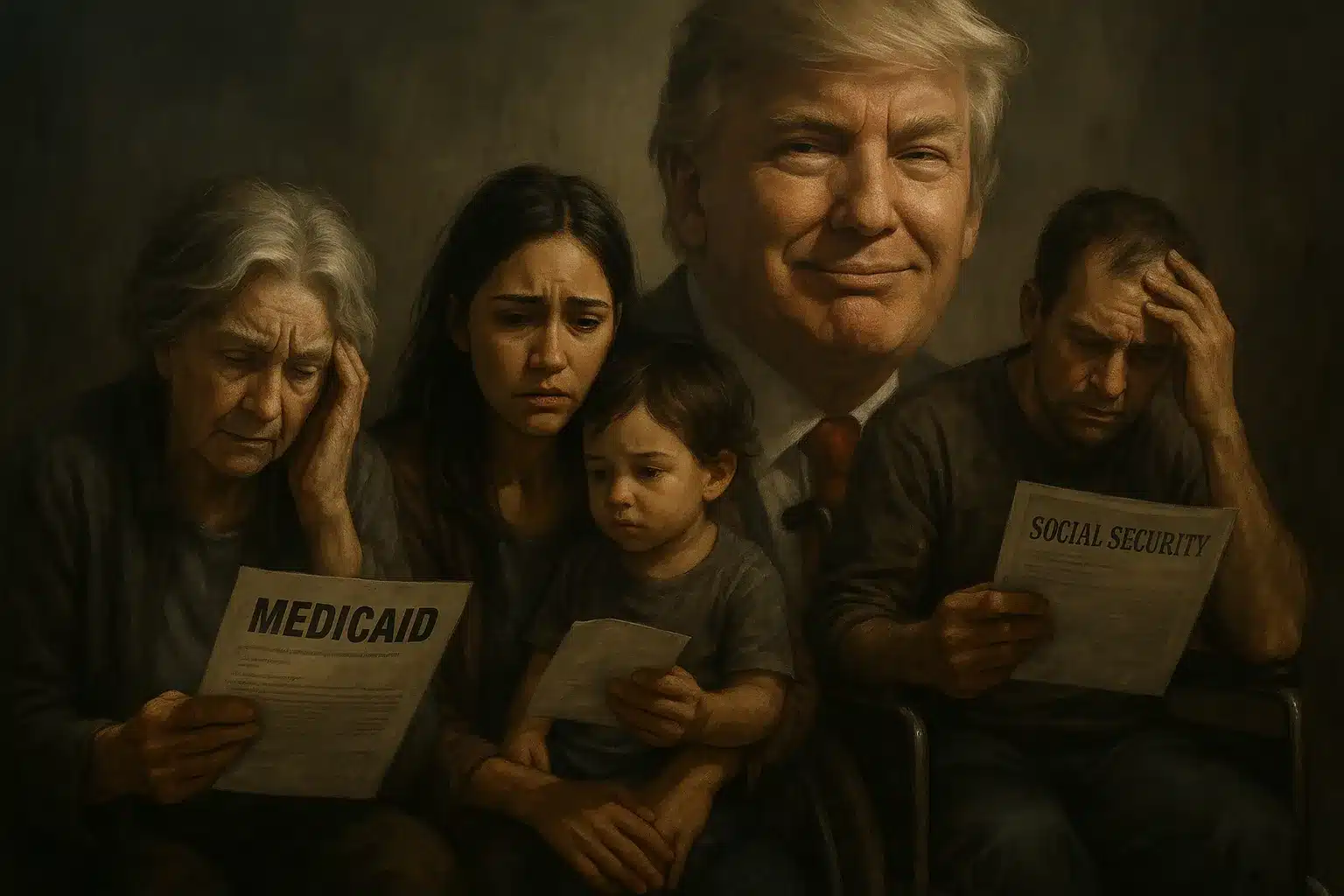
The Impact of Trump’s Tax Bill on Medicaid: A Closer Look
The recently signed federal spending bill by the Trump administration, heralded as the “One Big Beautiful Bill,” has raised significant concerns regarding its impact on Medicaid. With expected cuts exceeding $1 trillion over the next decade, the ramifications for low-income Americans, especially seniors, families, and people with disabilities, are profound.
What’s Changing Under the New Law
At the core of the new legislation are substantial alterations to Medicaid funding. While officials claim the bill prioritizes the most vulnerable populations, healthcare providers warn that the cuts may undermine essential services. Noteworthy provisions of the law include:
-
Work Requirements: Adults aged 19–64 must complete at least 80 hours of work monthly to remain eligible for Medicaid by December 31, 2026. Exemptions apply to pregnant women, individuals with serious health conditions, tribal members, and caregivers of disabled children.
-
Reduced Federal Reimbursements: A cut in federal reimbursements for hospitals and care facilities might hinder care access.
-
Stricter Eligibility Verification: Increased scrutiny over who qualifies for Medicaid can leave many eligible individuals without coverage.
- Frozen Support for Resource-Limited Facilities: Nursing homes and long-term care providers may face decreased financial support, impacting service availability.
Who Could Lose Coverage?
The introduction of work requirements is poised to affect millions. Historical evidence from Arkansas—where similar rules led to over 18,000 people losing coverage in just four months—suggests these requirements may disproportionately affect those in precarious employment situations.
As the policy analyst noted, “We’ve seen that administrative hurdles—even when small—can push eligible people off the rolls,” indicating the looming threat of loss of medial access for vulnerable populations.
Seniors and Disabled People Face Indirect Effects
While seniors and individuals with disabilities are exempt from these new work requirements, they are not immune to the adverse effects of Medicaid cuts. Crucially, around 65% of nursing home residents depend on Medicaid for their care. The program finances about 75% of long-term care expenses, making any cutbacks impactful.
With reduced reimbursements affecting healthcare facilities, potential outcomes may include staff shortages, decreased service quality, or even closures. Families may find themselves facing longer wait times and increased out-of-pocket expenses when seeking care for older or disabled relatives, further compounding health inequities.
Hospitals and Clinics Brace for Budget Stress
The law’s limitations on federal funding for provider assessments—often used by states to financially support Medicaid—raise alarms among health systems. Many organizations already battling operational deficits could find themselves in an untenable position, particularly in high-need, rural areas.
With an influx of Medicaid patients in these regions, the loss of funding could incite closures, mergers, or significant staff reductions, ultimately leading to diminished access to essential services.
What This Means for Patients
The overarching implications of these legislative changes could spell trouble for many Americans. Predictions indicate that nearly 12 million may become uninsured, transferring financial burdens onto those barely above eligibility thresholds.
Additionally, state governments might be pressured into hiking taxes or reducing funding for other vital programs to bridge the funding gaps created by these cuts, placing an overwhelming strain on public hospitals and clinics. As a result, patients may experience longer wait times and reduced quality of care as systems become overwhelmed.
As articulated by a national health advocate, “Medicaid supports more than just patients; it’s also the financial backbone of the safety-net system. When you cut Medicaid, you cut the infrastructure.”
What Happens Next?
The changes will roll out gradually, starting with work requirements in 2026 and reimbursement reductions extending through 2033. States face vital decisions on how to navigate these budgetary constraints—whether to increase spending or limit services.
Various health leaders, policy organizations, and advocacy groups are preparing to closely monitor the effects of these cuts. Some are even gearing up to challenge controversial aspects of the legislation in court, signaling ongoing political and legal battles over healthcare access in America.